Abstract
Background: more than 60,000 people die annually from hematologic malignancies in the united states (us). Patients with hematologic malignancies more frequently receive aggressive care toward the end-of-life and are more likely to die in a hospital compared to those with a solid tumor. Appropriate care of such patients is very dependent on an existing healthcare infrastructure. There are notable challenges to rural healthcare in the united states which contains less than 1/5th of all hospices in the us. In this study, we sought to investigate rural-urban disparities in place of death the us in individuals that died from hematologic malignancies.
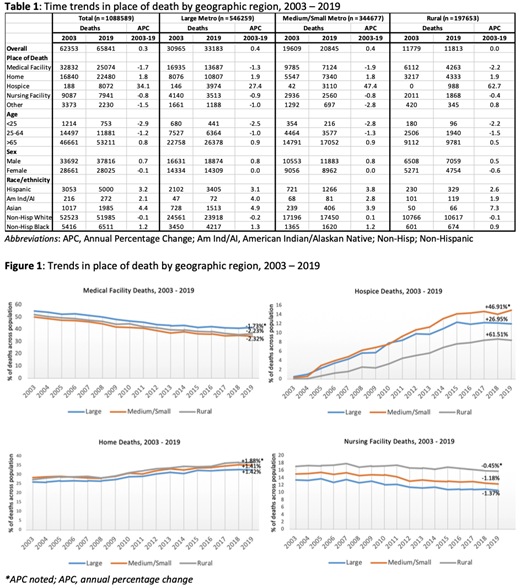
Methods: we utilized the us centers for disease control and prevention wide-ranging online data for epidemiologic research database to analyze all deaths from hematologic malignancies in the us from 2003 to 2019. A population classification utilizing the 2013 us census was made using the national center for health statistics urban-rural classification scheme. These classifications included: large metropolitan area (1 million), small- or medium-sized metropolitan area (50 000-999 999), and rural area (<50 000). We estimated deaths in a medical facility, hospice, home, or nursing care facility. We stratified the results by age, sex, and race/ethnicity. The annual percentage change (apc) in deaths was estimated. All data was publicly available and de-identified.
Findings: from 2003-2019, there were a total 1,088,589 deaths form hematologic malignancies in the united states, predominantly in large metropolitan areas (50.2%), followed by small or medium sized metropolitan areas (31.7%) and rural areas (18.2%). All regions noted decreases in medical facility and nursing facility related deaths, and increase in hospice and home deaths. While rural areas demonstrated the quickest uptake of hospice care (apc 61.5), they had the lowest overall presence of hospice care (8.3% of all rural deaths in 2019 vs. 14.9% for small or medium metropolitan vs. 12% for large metropolitan) and larger share of nursing facility related deaths (15.8% of all rural deaths in 2019 vs 12.3% for small or medium metropolitan vs 10.6% for large metropolitan).
Discussion: we demonstrate end-of-life disparities in hematologic malignancies based on where an individual resides in the us with rural areas having notably lower share of deaths in hospice facilities. Older infrastructure, inadequate access to care, and financial barriers add to the medical complexity of care for all patients, and especially hematologic patients with high needs and complex treatment planning. These have been aggravated by rural hospital closures in the previous 18 months. The us senate is currently debating a bipartisan infrastructure that may add billions in building rural healthcare infrastructure to state budgets. Our findings are timely in helping inform congressional policy.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal